Dr Ajay Kumar
The term non-alcoholic fatty liver disease (NAFLD), also known as hepatic steatosis (hepatic = liver, steatosis = fat), comprises a range of liver conditions where there is excess of fat in liver but without history of significant alcohol intake.
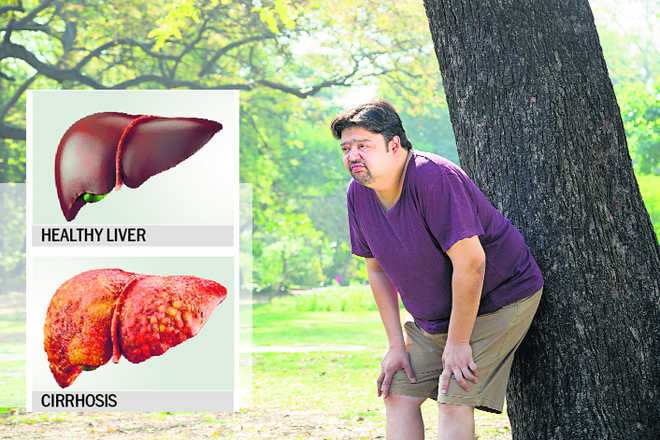
When heptic steatosis is associated with inflammation, it is called steatohepatitis(NASH). While steatosis is considered to be a mild problem and does not progress into serious disease, steatohepatitis is more likely to develop into complications of fibrosis and cirrhosis which can be serious, even fatal.
Non-alcoholic fatty liver disease is quite common and its incidence is increasing globally. It is commonly associated with those having metabolic syndrome and are possibly insulin resistant. These patients usually have type 2 diabetes, dyslipedemia (abnormal amount of lipids such as triglycerides, cholesterol and/or fat phospholipids in the blood) and hypertension and are obese. As India is the world capital of diabetes, NASH is also being seen in high proportion and is increasing every day. This has become a major reason behind liver cirrhosis in our country.
Non-alcoholic fatty liver disease can occur in any age but those in their forties and fifties are at more risk of having it. These are the people who are also in high-risk zone of having heart disease because of risk factors such as obesity and type 2 diabetes.
Symptoms
Usually, there are not many signs and symptoms of non-alcoholic fatty liver disease. The ones that are usually seen include:
- Enlarged liver
- Fatigue
- Pain in the upper right abdomen which is more like a dull ache
Complications
Cirrhosis of the liver can be a major complication associated non-alcoholic fatty liver disease and non-alcoholic steatohepatitis. It is the late-stage scarring (fibrosis) in the liver. Cirrhosis can be outcome of a liver injury such as the inflammation in case of non-alcoholic steatohepatitis. As the liver fights to prevent this inflammation, it produces areas of scarring (fibrosis). If the inflammation continues, fibrosis or this scarring spreads in the organ and replaces more and more tissue in the liver. Without timely interruption, cirrhosis can lead to:
- Buildup of fluid in the abdomen
- Veins in the oesophagus (oesophageal varices), can swell with possible risk of rupture and bleeding
- Confusion, drowsiness and slurred speech
- Liver cancer
- Liver failure, which means complete closing of the liver functioning
About 20 per cent of people with non-alcoholic steatohepatitis will end up getting cirrhosis of the liver.
Causes
What actually initiates this excess fat storage in liver is not clear. But many associations with this disease are well known such as:
- Overweight or obesity
- Insulin resistance which is usually associated with high blood sugar
- Presence of high levels of fats, particularly triglycerides, in the blood
These, combined with other health problems, appear to promote the deposit of fat in the liver. This excess fat acts as a toxin to liver cells for some people, causing liver inflammation and which may lead to a build-up of scar tissue (fibrosis) in the liver.
Prevention
There are certain preventive measures which can reduce the risk of non-alcoholic fatty liver disease. These include:
Healthy diet: Opt for a nutritious and balnced plant-based diet that’s rich in fruits, vegetables, whole grains and healthy fats.
Healthy weight: Maintain a healthy weight by consuming the number of calories you eat each day as per your weight and get more exercise. Work to maintain a healthy weight according to your height, age and gender by choosing a healthy diet and exercise daily.
Exercise: Get as much exercise as you can throughout the week. Consult with your doctor first for an adequate amount of work out according to your current health.
Six foods to avoid if you have a fatty liver
If you have fatty liver disease, there are some foods which you should definitely avoid or consume in a limit. These foods generally contribute to weight gain and increasing blood sugar which can be disadvantageous for you.
- Alcohol: Alcohol is an enemy of liver and a major cause of fatty liver disease as well as other liver diseases.
- Sugar: Foods such as cookies, sodas, juices, etc. should be avoided. High blood sugar can increase fat buildup in the liver.
- Salt: Excessive salt intake can make the body hold on to excess water. Salt should be limited to less than 1,500 milligrams per day.
- Fried foods: These are high in fat and calories without much nutritive value.
- Maida/refined flour: Avoid white bread, rice, and pasta. Most processed foods use refined flour which can raise blood sugar due to lack of fibre.
- Red meat: Red meat such as beef and deli meats are high in saturated fat.
— The writer is chairman & HoD, institute for digestive & liver diseases, BLK Super Speciality Hospital, New Delhi